Azoospermia Myths: What’s True and What’s Not?
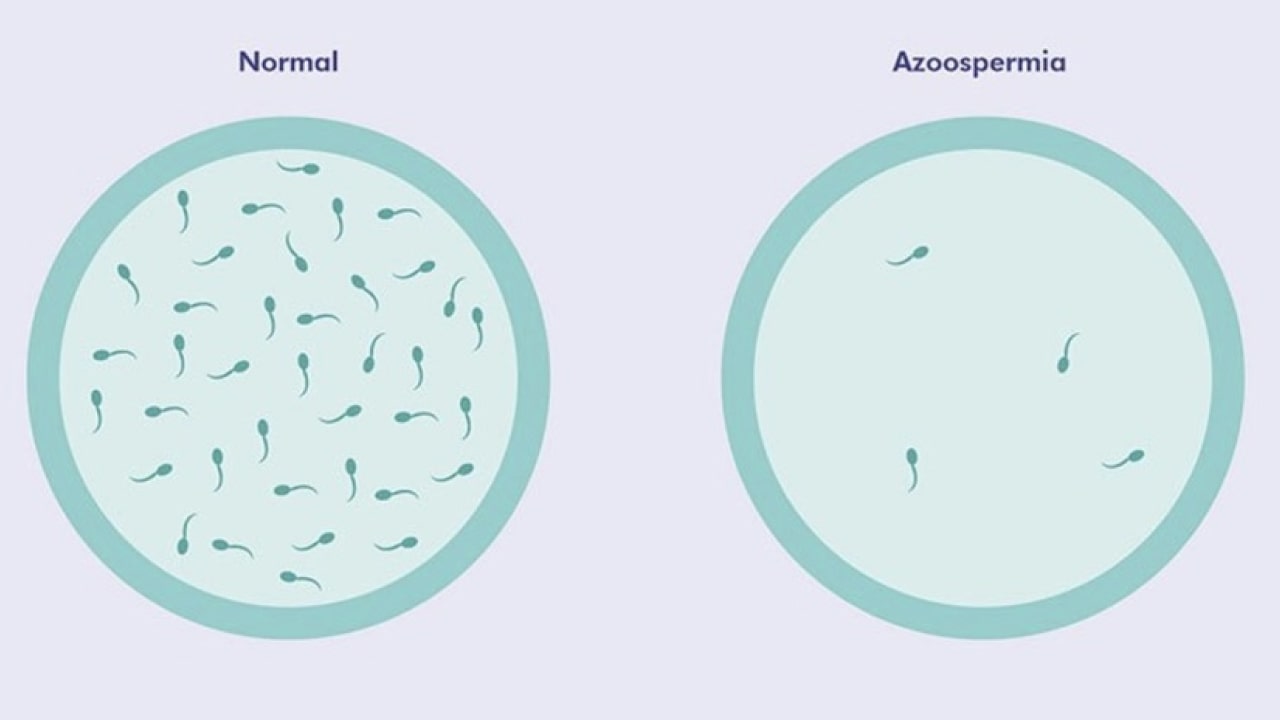
When it comes to male infertility, few conditions are as misunderstood as azoospermia. Characterized by the absence of sperm in semen, azoospermia affects roughly 1% of men and 10–15% of those seeking fertility treatment. Despite its prevalence, myths and misconceptions about the condition often leave couples feeling hopeless. Let’s separate fact from fiction and explore solutions like Sperm Plus tablets that may offer support.
What Is Azoospermia?
Azoospermia occurs when a man’s ejaculate contains no measurable sperm. It’s divided into two types:
- Obstructive Azoospermia (OA): Sperm is produced, but a blockage prevents it from mixing with semen.
- Non-Obstructive Azoospermia (NOA): The testicles produce little to no sperm due to hormonal imbalances, genetic issues, or lifestyle factors.
While the diagnosis can feel devastating, modern medicine offers hope. Let’s tackle the myths clouding this condition.
Myth 1: “Azoospermia Means You Can’t Have Biological Children”
The Truth: This is one of the most damaging myths. Many men with azoospermia can father biological children. In obstructive cases, sperm retrieved surgically (e.g., via TESE or micro-TESE) can be used in IVF with ICSI, where a single sperm is injected into an egg. Even in non-obstructive cases, sperm may sometimes be found in the testicles. Success rates vary, but parenthood is possible.
Myth 2: “Azoospermia Is Always Genetic”
The Truth: While genetic factors like Klinefelter syndrome or Y-chromosome deletions can cause NOA, many cases stem from reversible issues. Hormonal imbalances (e.g., low testosterone), infections, varicoceles (enlarged veins in the scrotum), or even prior surgeries (like vasectomies) may be to blame. Identifying the root cause is key to treatment.
Myth 3: “Lifestyle Choices Don’t Affect Sperm Production”
The Truth: Smoking, excessive alcohol, obesity, and exposure to toxins (like pesticides) can harm sperm production. Studies show that men who adopt healthier habits—like quitting smoking, reducing stress, and eating antioxidant-rich diets—often see improved sperm quality. While lifestyle changes alone may not cure azoospermia, they can enhance overall fertility.
Myth 4: “Azoospermia = Infertility”
The Truth: Infertility is a broad term, but azoospermia is a specific diagnosis. Some men with azoospermia still have viable sperm in their testicles. Even if natural conception isn’t possible, assisted reproductive technologies (ART) like IVF/ICSI bridge the gap.
Myth 5: “There’s No Treatment for Azoospermia”
The Truth: Treatment depends on the type and cause:
- Obstructive Azoospermia: Surgery to repair blockages (e.g., vasectomy reversal) or sperm retrieval for IVF.
- Non-Obstructive Azoospermia: Hormone therapy (e.g., Clomid), varicocele repair, or experimental treatments like stem cell therapy.
Even if sperm retrieval fails, donor sperm or adoption remain options.
Sperm Plus Tablets: Can They Help?
Amidst the confusion about azoospermia, many turn to supplements like Sperm Plus tablets to boost fertility. Let’s break down what they are and whether they work.
What Are Sperm Plus Tablets?
Sperm Plus is a dietary supplement formulated to improve sperm count, motility, and morphology. Common ingredients include:
- Antioxidants (Vitamins C, E): Combat oxidative stress, a known sperm killer.
- Zinc and Selenium: Essential for testosterone production and sperm development.
- Herbal Extracts (Ashwagandha, Mucuna Pruriens): Shown in studies to enhance sperm parameters.
Do They Work for Azoospermia?
While Sperm Plus isn’t a cure for azoospermia, it may support overall reproductive health:
- For Mild Cases: Men with low sperm counts (oligospermia) may see improvements in count and motility.
- Pre-Surgical Support: Boosting sperm health before retrieval procedures could enhance IVF success.
- General Wellness: Reducing oxidative stress benefits overall fertility.
Important Note: Always consult a doctor before starting supplements, especially with azoospermia. They’re not a substitute for medical treatment.
The Emotional Side of Azoospermia
Beyond the physical challenges, azoospermia can strain relationships and self-esteem. Open communication with your partner and counseling can help. Remember: Infertility is a medical condition, not a reflection of masculinity.
Final Thoughts: Hope and Next Steps
An azoospermia diagnosis isn’t the end of your parenting journey. Advances in reproductive medicine, combined with lifestyle tweaks and supplements like Sperm Plus, offer tangible hope.
Next Steps:
- Consult a Specialist: A reproductive urologist can pinpoint the cause and recommend treatments.
- Explore ART: IVF/ICSI with retrieved sperm has helped countless couples.
- Consider Supplements: Discuss options like Sperm Plus with your doctor.
Infertility is a tough road, but you’re not walking it alone. By debunking myths and embracing science-backed solutions, parenthood may still be within reach.
Also read:
Lifestyle Changes That May Help with Azoospermia




Leave a Reply